
An example of a human resource error is not enough anaesthetists available to attend a crisis in another theatre during a normal working day. Some pumps have multiple steps to their programming, making it difficult to check the correct data have been entered. 2), and the wrong drug or concentration could easily be administered. 8–10 For example, many drugs have similar packaging (see Fig. They are the factors that have contributed to the event. These errors tend to be ‘systems’ related.
These errors are wide ranging-the building/room layout, organizational processes, human resources, equipment failure, or medication error.

They do not directly cause the error and occur upstream of the event. Latent errors occur at the ‘blunt end’ of health care. Active errors are usually picked up quickly at the time of the incident and therefore more easily identified. Examples include an anaesthetist administering an incorrect drug dose to a patient or not turning on the oxygen flow for pre-oxygenation in a rapid sequence induction of anaesthesia. 8, – 10 These errors tend to be person/individual related or immediate equipment failures. 1).Īctive errors occur at the ‘sharp end’ of health care, where an action directly causes an error in real time. violations and malevolent acts.Įrrors can be thought of as active or latent ( Fig. The conscious movement away from established rules within an organization, i.e.
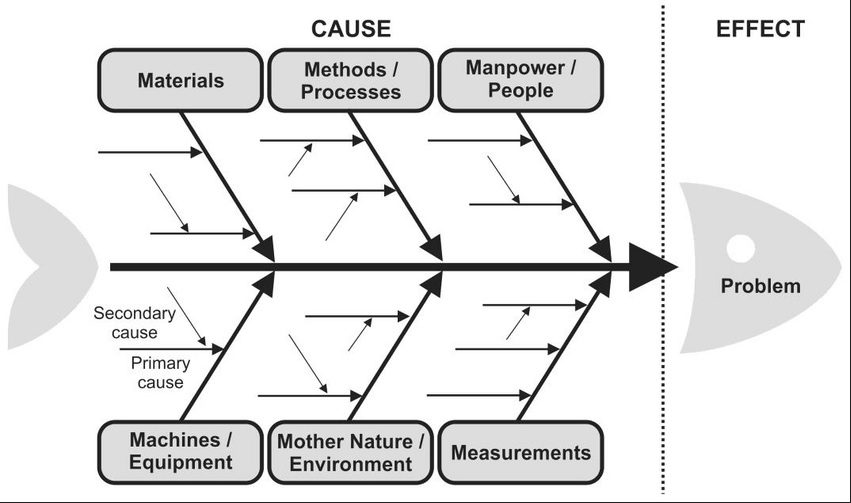
The thought process related to the error, poor planning, or poor execution of a task. The time point the error occurred relative to the error identification, i.e. 2 Fortunately, not all errors lead to actual patient harm.Įrrors can be classified according to: 8, 9 ErrorsĮrrors can be defined as an act of commission or omission leading to an undesirable outcome or potential undesirable outcome. This article explores the theory of error occurrence and systems we use to learn from it. Patient safety was further highlighted by the Elaine Bromiley case in 2005. Anaesthesia was one of the first specialities to introduce patient safety guidelines into practice. Reason’s work forms the basis of the rapidly expanding field of patient safety. As health care has evolved over time, so has our understanding of error and its management. But how do we reconcile this with modern health care, where safe effective patient care is the pinnacle of our practice? James Reason, a British psychologist, founded the framework of error classification and management in health care in the 1990s. This might include an inaccurate or incomplete diagnosis or treatment of a disease, injury, behaviour, infection, or other ailment. Specifically, a medical error is a preventable adverse effect of care, whether or not it is evident or harmful to the patient. Cognitive psychologists believe that slips, lapses, and mistakes are inevitable, as they are the price we pay for advanced higher cerebral function. Everyone makes mistakes it is part of the human condition. ‘Knowledge and error flow from the same mental sources, only success can tell one from the other.’ 1Īn error is an act that can lead to an undesirable outcome. Root cause analysis is a systematic process whereby the factors that contribute to an incident are identified and learned from. In the NHS, incident reporting systems are a form of voluntary staff-led error data collection and collation. Errors can be defined as an act of commission or omission leading to an undesirable outcome or potentially undesirable outcome.Įrror can be classified as active or latent, individual or system based.Īddressing the individual error may prevent the person repeating the same error, whereas addressing latent errors and contributing human factors may prevent an entire organization from making the error again.


 0 kommentar(er)
0 kommentar(er)
